 One of the most common questions I get from clients and readers alike is "how can I fix my gut?"
One of the most common questions I get from clients and readers alike is "how can I fix my gut?"
The answer is anything but simple because it depends on what is going on in your gut. And there are a lot of possibilities and combinations, like:
- Liver and biliary issues (at the top of the list for a reason because it can 'set the stage' or allow most of the following to occur in the first place)
- Bacterial pathogens
- Parasitic pathogens
- Viral pathogens
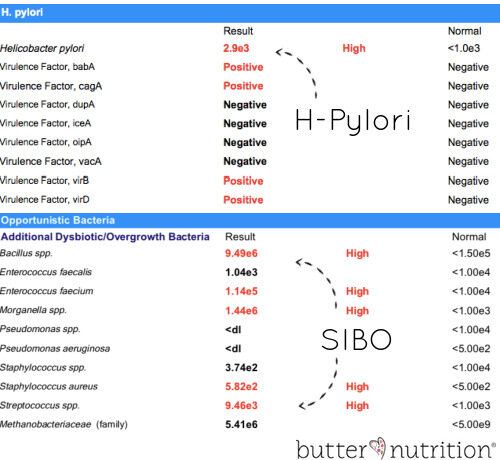
- H-pylori
- Disruption of normal bacterial flora
- Imbalance of phyla microbiota
- Overgrowth of opportunistic bacteria
- Parasites
- Fungi/yeast
- Viruses
- Worms
- Food allergies
- Hypothyroidism
*Most of the above are tested on the extensive GI Map stool test that I use with my clients (sample results can be found here).
Gut health and gut healing protocols often seem confusing, expensive and complicated. Today I hope to shed light on what is behind a good gut healing protocol and how to best go about finding the next course of action in fixing your own gut.
When I speak of gut problems, I'm generally talking about a mix of the following symptoms:
- Belching or gas within one hour after eating
- Heartburn or acid reflux
- Histamine intolerance
- Feeling bloated within one hour after eating
- Bad breath
- Loss of appetite
- Stomach upset by taking vitamins
- Feel like skipping breakfast/feel better when you don't eat
- Sleepy after meals
- Fingernails chip, peel, break, or don't grow
- Anemia unresponsive to iron
- Stomach pains or cramps
- Chronic diarrhea or shortly after meals
- Chronic constipation
- Undigested food in stool
- Estrogen dominance symptoms (namely weight gain around hips/thighs, breast tenderness, more here)
Incredibly unpleasant and life-sucking, right? Believe me, I know.
How gut issues start
Why do these kinds of issues start in the first place? The reasons for gut issues are endless, but here's some of the most common triggers:
- Liver problems and biliary stasis - when the liver and biliary system isn't able to do its job of filtering and removing toxins from the body, toxins can re-circulate and build up in the body. When the liver and biliary axis is overwhelmed by toxins it impacts the digestive environment in a number of unfavorable ways. You see, bile is produced in the liver and stored in the gallbladder. Then it is released when you eat a meal to aid in the digestion of fats as well as the digestive process. Bile not only helps to emulsify your fats for digestion, but it also helps with peristalsis or motility, and acts as an antimicrobial substance to help keep your digestive tract clear of bacterial overgrowth.
- H-Pylori - a H-pylori overgrowth decreases stomach acid and opens the door to what I call "gut chaos". And by gut chaos, I mean it opens the door for pathogens, bacteria, viruses and more to overgrow in your gut. This is because stomach acid (often called hydrochloric acid or HCL) is the protector of your gut. If it's production is insufficient or compromised by H-Pylori bacteria your gut can become something like an open-door house party for any invader.
How do you get H-Pylori? You can get it from drinking water. About 50% of the population has H-Pylori in their stomach, but it may not be a problem if your immune system and gut are balanced and can keep growth at bay. - Motility issues from liver/biliary stasis and/or:
- Dietary changes - drastic changes in your diet set the stage for serious changes in your gut microbiome. One big example I see is when someone shifts from a normal diet to a low carbohydrate, ketogenic or carnivore diet. You see, your good gut bacteria need proper food to survive and they really like fiber (fruits, veggies, non-gut irritating fiber supplements) and polyphenols (green tea, blueberries, cranberries, etc.) So if you all the sudden take out all the fiber and polyphenols to just eat meat, your good gut bacteria can commit suicide letting the bad bugs prosper and overgrow leading to something called small intestine bacterial overgrowth (SIBO) or large intestine bacterial overgrowth (LIBO). While some studies and carnivore dieters claim fiber-free diets can have a positive impact on your gut biome, that's just not what I see in my own practice, and I think it's more person/genetics specific. There is a huge genetic component to gut health. Drastic dietary changes also tend to cause constipation, which can set the stage for bacteria overgrowth due to lowered gut motility.
- Dieting - restriction of food or calories in the diet can slow gut motility creating the perfect conditions for overgrowth as well as cause nutritional deficiencies that can impact hydrochloric acid production (again talking about stomach acid because it is so important!) [3,4]
- Chronic stress - when your body is stressed, it's focused on survival and digestion is down regulated to re-direct energy to other areas of the body since surviving stress is prioritized over digestion. This means less digestive juices to digest food properly, causing you to assimilate fewer nutrients. Chronic stress also impacts the immune system and the ability your gut has to keep pathogens under control.
- Antibiotic use - antibiotics not only kill off the intended target but also can reduce levels of beneficial bacteria. This then allows pathogenic or opportunistic bacteria the chance to grow and overgrow.
- Food poisoning - a large influx of pathogenic bacteria in a susceptible gut can spark overgrowth conditions if your immune system is suppressed.
- Aging - stomach acid can naturally decline with age increasing the probability of gut-related issues.
- Proton pump inhibitors - PPIs turn off stomach acid disrupting an important part of the digestive process. Stomach acid's job is to kill off bacteria and pathogens as they come in your body through your mouth. If the stomach acid is reduced, it's going to cause downstream issues in the digestive tract.
Often someone with chronic gut issues has a combination of these triggers. For instance, H-Pylori is commonly seen with small intestine bacteria overgrowth (SIBO) and large intestine bacteria overgrowth (LIBO). The longer the gut issue has been going on, the more likely there is a bigger overgrowth party going on in the gut.
How to Fix Your Gut
When you start off on the journey to fix your gut, having data on your gut really helps (I use a GI Map and/or Organic Acid test in my clients to assess their gut terrain). Sure there are some generic things you can do, which I will talk about, but it really helps to know exactly what is invading and/or overgrowing in your gut, so you know how to approach it with accuracy instead of just guessing.
Guessing can be even more expensive than testing, because many of these gut supporting supplements are not cheap (and if you use the wrong ones you can also exacerbate bloating and discomfort). You only want to use what is indicated and needed to get the best results while spending the least amount of cash money (as my nephews call it).
Upstream and Downstream Factors
There are two main ways I like to look at gut issues - upstream and downstream.
- Upstream looks to address the communication between the brain and the gut via the vagus nerve, the liver/biliary system, cellular inflammation, and cellular energy production.
- Downstream is the most typical approach, addressing what is going on in the gut and supporting what needs to be supported.
It's important to address both upstream and downstream gut issues. For instance, a common cause of upstream digestive dysfunction is an impaired migrating motor complex (MMC) that is super important for gastrointestinal (GI) contractions that help move your food through your digestive system. A slowed MMC can trigger bloating, constipation and bacterial overgrowth simply by a decrease in digestive motility due to insufficient communication from the brain.
An upstream approach would address - why isn't the MMC doing its job? Are nutritional deficiencies impairing cellular energy production? Is there cellular inflammation that needs to be addressed first? Is the client eating enough food to support proper thyroid health?
A downstream approach would support peristalsis, address overgrowth, and get the bowels moving in one way or another.
Sometimes if you fix the problems upstream, the gut can repair itself without a lot of dietary and supplemental intervention needed. This is always my goal, but it often boils down to a combination of support on both ends.
There are 3 main stages to fixing your gut:
Each practitioner has their own approach, so this will vary slightly (order and includes) by who you work with, but these are the common basics.
Stage 1: Change the digestive environment
Stage one is all about diet and setting the stage to change your digestive environment (that allowed the situation to occur in the first place).
Things that are therapeutic here are things like:
- Diet - generally speaking, is your diet adequate?
- Are there foods, supplements and toxins in your diet that are overwhelming your liver and perhaps the root cause of the problem?
- Are you eating enough protein to get vital minerals and support detoxification by supplying adequate amounts of amino acids?
- Probiotics - to encourage gut diversity and knock down opportunist bacteria loads. The type of probiotics is confusing, as different strains are therapeutic for different conditions. Some of my favorites are:
- Lactobacillus Reuteri can be helpful in cases of H-Pylori and Clostridioides difficile [5]
- Saccharomyces Boulardii has been shown to be helpful in some SIBO cases, specifically more diarrhea prone cases
- Lactobacillus and Bifidobacterium strains
- Spore based probiotics
It's important to remember that all probiotics were not created equal and certain probiotics are helpful to some and disastrous in others. Again, knowing what is going on in your gut can help narrow your support options.
Something else I think is incredibly, incredibly important for stage 1 is fatty acid balance (omega-6:omega-3 and your AA:EPA ratio). If your fatty acid imbalance is off, it can cause cellular inflammation, and that can make fixing your gut an uphill battle.
Stage 2: Support digestion, liver/gallbladder, pancreas function and calm inflammation (organ + digestive support)
If you get a GI Map (stool test) done, your results will indicate if you need digestive, gallbladder, pancreas, immune or anti-inflammatory support through markers like elastase-1, secretory IgA, steatocrit and calprotectin.
This support category includes things like bitters, bile support (super important), digestive enzymes, immunoglobulins (one of my favs), butyrate and more to help support proper digestion and calm down any inflammation present. Again, data helps narrow down what exactly you need to be best supported. But let's break down what each of these do a little further...
Digestive Enzymes - can be either plant or animal based and contain enzymes to help you break down your proteins, carbohydrates and fats when your body is not producing adequate amounts.
Bitters - digestive bitters have been around a long time. They are typically herbal concoctions that are taken before meals to help stimulate stomach acid as well as bile so that you can properly digest your food and absorb nutrients.
Beets - While I've probably talked about my love of beets and beet juice all over the blog for gallbladder support, they really do a great job at helping to thin bile flow which helps keep your digestive tract moving, clean, as well as supports toxins leaving your body.
Serum Bovine Immunoglobulins - immunoglobulins are one of my very favorite gut support products (they are a "support" and not an intervention). Immunoglobulins are immune proteins extracted from bovine blood and act like police in your gut. They bind and deactivate bacteria, pathogens and toxins so they can't do more harm. I love using them in my gut protocols because they help to lessen inflammation while binding to bad guys and escorting them out of the body. They are also used on a higher dose more therapeutic level in cases of chronic diarrhea. Research can tell a great deal about the value of immunoglobulin - "Numerous studies have demonstrated that oral administration of plasma- or serum-derived protein concentrates containing high levels of immunoglobulins can improve weight management, normalize gut barrier function, and reduce the severity of enteropathy in animals." Enteropathy refers to the pathology of the intestine, for reference. [8]
Lactoferrin - is another kind of immune protein. Lactoferrin is found in mammillary milk and has antimicrobial, anti-inflammatory and immunomodulatory properties. [13] Lactoferrin and immunoglobulins are the important immune-regulating proteins found naturally in colostrum products, but can also be found in isolated form.
Butyrate - is something called a short-chain fatty acid (SCFA). Certain bacteria are what we call butyrate producers. In short, fiber is their fuel source and they use it to create butyrate and other SCFA which becomes fuel for your colon cells. This is extremely important because your colon cells need enough butyrate to keep your colonic mucosal barrier healthy which protects you from inflammation.
Peptides (specifically BPC-157, BPC= Body Protection Compound) - peptides are signaling molecules that can help with regeneration, brain inflammation and be incredibly therapeutic in gut issues. BPC-157 is a gastric juice peptide that can help with gut brain communication in the body as well as gut healing. [9,10,11]
Prokinetic agents - prokinetic agents help gastrointestinal motility by supporting the strength of contractions in the digestive tract. They are particularly important in gut issues involving chronic constipation. Some common prokinetics are:
- Ginger
- Motilpro
- Iberogast
- Triphala
Stage 3: Support a healthy gut by feeding your good bacteria
Stage three is all about diet and helping to make sure your healthy gut bacteria have a 5-star meal every day to keep them thriving. You see, often you can counteract bad bacteria overgrowth in a subtle and gentle way by just letting your good bacteria grow and crowd out the bad guys. This is always the preferred way to go, so typically it is the first step and is given some time to see how your body responds (everyone's gut is different).
Things that are therapeutic here are things like:
- Prebiotics - fiber-rich prebiotic foods provide food for your good gut bacteria to thrive. While prebiotic fibers can be an amazing way to support altering your gut microbiome, there are certain types of prebiotics and conditions where fiber is not tolerated well. Common prebiotics are:
- Fibers found in fruits/veggies, especially oats, beans and whole grains (if tolerated)
- Inulin/resistant starch
- Galactooligosaccharides (GOS)
- Fructooligosaccharides (FOS)
- Partially Hydrolyzed Guar Gum (PHGG)
- Lactulose
- Human milk oligosaccharides (HMO)
- Polyphenols - foods like green tea, blueberries, cranberries, beans, etc.
Stage 4: Reducing the bad bugs if still needed, this is a last resort
The forth stage typically involves herbal microbial agents, antibiotics (typically the route mainstream doctors will take), biofilm disruptors (lumbrokinase, nattokinase are some of my favs) and other natural (or unnatural) interventions to aid in reducing unwanted pathogens. Sometimes, this you can avoid this stage all together by just changing the terrain in your gut to make it inhospitable to bad critters and supporting any organs under stress. It's all so person specific and depends on what kind of bacteria party is happening in your own gut.
According to my evolving body of knowledge on this topic, it actually can be counterproductive to use antimicrobials, especially too early or for too long because of the impact they can have on the gut microbiome as a whole. When I do use them, I typically choose the gentlest ones and use them for a short period of time that is only deemed necessary by testing. Some of my favorites are:
- Allimax
- Berberine
- Mastic gum
- Monolaurin
- Neem
Whether or not you need stage 1, 2, 3, 4 or all of them depends on what is going on in your gut per testing, and how your body reacts and changes in response to interventions given.
Dietary Changes
Often special diets are done in addition to the stages above. It really just depends on the practitioner you are working with and what they find works best with their clients.
If testing is not in the budget for you or you're just not interested in that route, there are some therapeutic diets that can help decrease symptoms but they can be limiting, and involve a lot of trial and error, especially if you go it on your own. These diets include:
- The Simple Carbohydrate Diet (this is my personal favorite)
- FODMAPS
- Gluten free diets
- Dairy free diets
- Grain free diets
Note: these diets are NOT intended to be done for an extended period of time. While these can be incredibly helpful for providing quick relief, they often do not solve the underlying gut issue, and the issues may return. Dietary changes are best done in combination with a solid gut support protocol designed for you.
While this post barely scratches the surface of gut healing, I hope it helps demystify gut healing protocols and helps you understand new possible steps and/or a direction for your own gut healing journey.
How to Build a Bulletproof Gut Masterclass
This is a paid online digital masterclass with the information spread out over 2-3 days.
I'll be sharing things I CAN'T share in a public place like:
- The exact process I go through with my clients to improve their gut 🚀
- The exact supplements, supports and food-based approach I use to change the gut environment 🔬
- All my favorite probiotics, prebiotics, postbiotics, motility support and therapeutic foods (and how I use them) 💊
- The liver and gallbladder connection to chronic gut issues 💀
- Recommended testing and more!
So if you're:
...eating well
...doing everything 'right'
...but STILL having gut symptoms and not sure what step to take next, this masterclass will inform you, empower you, and accelerate your results without the high cost of working one-on-one 🚀🚀🚀 Join the gut-changing masterclass here.
And as Hippocrates so wisely said, "All disease begins in the gut.
PIN IT:
References:
- https://www.diagnosticsolutionslab.com/
- https://matrixhealthwell.com/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5609274/
- https://link.springer.com/article/10.1007/s12328-015-0611-x
- https://pubmed.ncbi.nlm.nih.gov/31174707/
- https://drruscio.com/3-best-probiotics-of-2020-how-to-use-them-effectively/
- http://www.hormonesmatter.com/thiamine-deficiency-causes-problems/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4041178/
- https://pubmed.ncbi.nlm.nih.gov/29879879/
- https://pubmed.ncbi.nlm.nih.gov/27138887/
- https://pubmed.ncbi.nlm.nih.gov/28228068/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5751248/
- https://www.frontiersin.org/articles/10.3389/fnut.2021.759507/full






Rebecca Barker says
Hi Catherine,
Now that genetic testing is available for dietary support, like joinzoe and genopalate, do you have an opinion about how they might be beneficial as an addition to your programs? It seems to me it might be a waste of time to pursue them before a GI Map test if one has gut issues because the recommendations might not be helpful in the short term if they are not doable.
Catherine says
Hi Rebecca,
Genetic testing only tells you your 'genetic potential.' It doesn't tell you if those genes are expressing in a problematic way in the now, so that's why I like more 'real time' data to see what is actually manifesting.
Abundantly,
Catherine
Carol says
Hi,
I have intestinal problems, chronic constipation,
Gain weight, inflation bloating, I dont how stop that.One day a doctor told me maybe I have bugs
But I don't onow how to kill them.